 After Starting HUMIRA® for Ankylosing Spondylitis
After Starting HUMIRA® for Ankylosing Spondylitis301 Moving permanently Biologics and Crohn's Disease Remission: What You Need to Know OverviewIn 1932, Dr. Burrill Crohn and two colleagues presented a document to the American Medical Association describing the details of what we now call Crohn's disease. Since then, the treatment options have evolved to include the biologics, which are medicines made from living cells that are designed to point the inflammation. Inflammation is the main cause of the symptoms and complications of Crohn's disease. When you're in remission, your inflammation fades. When you're experiencing a Crohn's bengala, your inflammation returns. Although there is no cure for Crohn, the goal of treatment is to reduce inflammation to put the disease in remission, and keep it there. The tumor necrosis factor, or TNF, is a protein that induces inflammation as part of an immune system response. Anti-TNF biologics work by targeting this protein to reduce its inflammatory properties. If you take Remicade (infliximab), Humira (adalimumab), Cimzia (certolizumab), or Simponi (golimumab), you are taking an anti-TNF biologic. With Crohn's disease, his immune system sends too many white blood cells to the gastrointestinal tract (GI), which triggers inflammation. Another way that biologicals are directed to inflammation is by addressing the problem of having too many white blood cells in the GI tract. Entyvio (vedolizumab) and Tysabri (natalizumab) work this way. They stop the white blood cells from entering the stomach. This blocking action keeps white blood cells away from the intestine, where otherwise they would cause inflammation. In turn, this allows the area to heal. Biologicals may point to other pathways in the body leading to inflammation. Stelara (ustekinumab) is an interleukin inhibitor. It targets two specific proteins that are believed to cause inflammation. People with Crohn have higher levels of these proteins in their body. By focusing these proteins, Stelara blocks inflammation in the GI tract and decreases symptoms of Crohn's disease. It's normal to have good days and bad days when you have Crohn's, so how do you know if you're in remission and not just have several good days? There are two aspects for remission. Clinical referral means that you have no notable symptoms. The tissue remission means that the tests indicate that your injuries are healing and your blood has normal levels of inflammation. Your doctor uses something called Crohn's disease activity index (CDAI) to measure the extent to which your Crohn is active or in remission. CDAI takes into account its symptoms, such as the number of intestinal movements and how it feels. It also takes into account the complications of Crohn's disease and the results of its tests. Even while you are in remission, it is common for a biopsy to show microscopic changes in your tissue that indicate previous inflammation. Sometimes, in the case of prolonged and deep remission, the results of the biopsy are normal, but this is not usually the case. Biologicals keep you in the remission by blocking the hyperactive inflammation response of the immune system. If you leave your medication while you are in remission, you are more at risk of reacting to a trigger with a flare. Sometimes triggers can be hard to predict. Others, such as the following, are easier to identify: If you are taking medications while exposed to triggers, Crohn's disease is less likely to be activated. Biosimilars are later versions of biologicals with very similar structure, safety and effectiveness. They are not generic versions of the original biologicals. Instead, they are copies of original biologicals whose patents have expired. They usually cost less and are also effective in maintaining remission. Once you are in remission, you can be tempted to stop treatment. If you do, you run the risk of experiencing a new flare. If you stop taking your medication, there's a chance that it won't work so well next time you have a flare. This is because when you stop taking a biologic, your body can grow antibodies against the medication, which makes it less effective in the future. It could even lead to adverse reactions. Biologicals suppress your immune system, which puts you at risk for infection. Because of this, there are certain situations in which your doctor may advise you to take a break from the medication. These include: Otherwise, the recommended practice is to stay in the medication even when you are in remission. Studies have shown that only about half of the people who stop using their anti-TNF biologics while in remission they actually remain in remission for more than two years, and that number decreases over time. The goal for the treatment of your Crohn is to obtain and maintain remission. Lost medication can cause flares. It is important to work with your doctor to establish the best strategy to stay in remission. This includes having regular checks and keeping your medication regimen. Last medical review on February 27, 2019Read more here
Sorry for our Interruption As you were browsing something about your browser made us think it was a bot. There are a few reasons why this could happen: To recover access, make sure cookies and JavaScript are enabled before reloading the page. After completing the CAPTCHA then you will immediately recover access to the site again.
:max_bytes(150000):strip_icc()/is-it-safe-to-drink-alcohol-with-humira-4175593-v2-b647651859464347831364eeb1d2792c.jpg)
Risks of Consuming Alcohol With Humira
Ankylosing Spondylitis & HUMIRA® (adalimumab)
What to Expect with HUMIRA® (adalimumab) for HS Treatment
2021 PDR, LLC. All rights reserved. < Back PDR.net Advertisement HUMIRA- adalimumab HUMIRA- adalimumab injection, solution AbbVie Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information ...
HUMIRA® (adalimumab) | A Biologic Treatment Option
What to Expect with HUMIRA® (adalimumab) for HS Treatment
Taking Citrate-Free Humira: What Patients Need to Know
HUMIRA® (adalimumab) Citrate-free Injection
HUMIRA® (adalimumab) Cost, Copay, and Savings Card
Managing Rheumatic and Immunocompromised Diseases During COVID-19
How HUMIRA® (adalimumab) Treatment Works for RA
Makers of Humira and Enbrel Using New Drug Patents to Delay Generic Versions - The New York Times
Adalimumab | Crohn's & Colitis UK
Immunosuppressing Medications for Inflammatory Conditions During the Coronavirus Pandemic
HUMIRA® (adalimumab) | For Healthcare Professionals in Rheumatology
Humira: Side effects, cost, uses, and more
Register for Plaque Psoriasis Information | HUMIRA (adalimumab)
Humira (Adalimumab Injection Solution for Subcutaneous Administration): Uses, Dosage, Side Effects, Interactions, Warning
Learn About STELARA® (ustekinumab) for Crohn's Disease | STELARA®
HUMIRA Dosing Information | Injection for Plaque Psoriasis
Adalimumab | Crohn's & Colitis UK
Crohn's Remission and Results With HUMIRA® (adalimumab)
ADALIMUMAB (Humira)
Active Ankylosing Spondylitis | HUMIRA® (adalimumab)
Humira (Adalimumab Injection Solution for Subcutaneous Administration): Uses, Dosage, Side Effects, Interactions, Warning
Crohn's Remission and Results With HUMIRA® (adalimumab)
Common Questions About Taking Methotrexate for Rheumatoid Arthritis
Humira 40 mg/0.4 ml Pre-filled Syringe and Pre-filled Pen - Summary of Product Characteristics (SmPC) - (emc)
Humira (Adalimumab Injection Solution for Subcutaneous Administration): Uses, Dosage, Side Effects, Interactions, Warning
Humira (Adalimumab Injection Solution for Subcutaneous Administration): Uses, Dosage, Side Effects, Interactions, Warning
Main Header
ADALIMUMAB
Adalimumab (Humira®)
6 Things to Expect If You Take Biologics for Crohn's
Humira: Side effects, cost, uses, and more
Stopping and Restarting Biologic Medications for Psoriasis
Humira CMI for Pre-ADEC
Immunosuppressants and Coronavirus: Here is What You Should Know
Biologics and Remission in Crohn's Disease: What You Need to Know
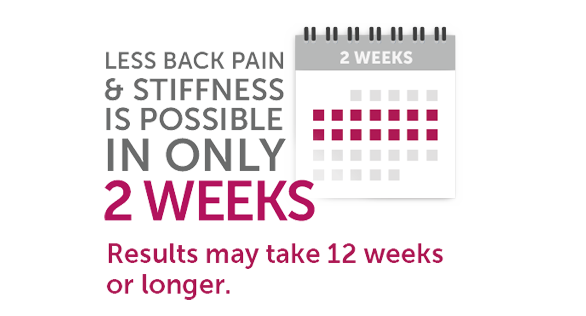 After Starting HUMIRA® for Ankylosing Spondylitis
After Starting HUMIRA® for Ankylosing Spondylitis:max_bytes(150000):strip_icc()/is-it-safe-to-drink-alcohol-with-humira-4175593-v2-b647651859464347831364eeb1d2792c.jpg)

























Posting Komentar untuk "what happens when you stop taking humira"