 Nursing Care Plan For Newborn Baby - Newborn baby
Nursing Care Plan For Newborn Baby - Newborn babyLippincott ® Low weight of infants consummation, risks and interventions Source:Infants " Young ChildrenJuly 2002, Volume :15 Number 1 , page vi - ix [Free] to obtain uninterrupted access to this article Authors Contents Of the approximately 4 million live births per year in the United States, 7.5% are classified as low birth weight (LBW, thanks to the latest perinatal services and the incredible advances in neonatal intensive care technology (approximately 700 tertiary neonatal intensive care units [NICUs] in the United States), the overwhelming majority of the youngest and most ill children who now survive. The regionalization of perinatal care with maternal transport to highly specialized centres, often referred to as level III facilities, has had a significant impact on supporting the survival of LBW, premature babies. 90% and higher survival rates are currently the expectation of up to 1,000 grams (28 weeks of gestation) with very low-weight infant rates (ELBW, The growing survival of fragile premature babies has, fortunately, produced a strong interest in defining their long-term results, identifying their "quality of life," and investigating intervention strategies to improve their development/behavioral prognosis. The neurodevelopment result of LBW infants can be conveniently divided into topics of so-called "major" and "minor" impediments. Among the main impediments are disabilities such as cerebral palsy, delays in global development (mental retardation over time), epilepsy, hearing and/or visual loss, and progressive hydrocephalus. These impediments tend to be more severe (although they certainly have milder forms), identified in the first two years of life, and caused by substantial brain insults such as hemorrhage or hypoxia/ischemia. They often occur more often in lower birth weights and gestational ages, and have identifiable markers in the neuroimagen. Approximately 15-20% of VLBW survivors and 20-25% of ELBW survivors will develop one or more important neurodeveloped deficiencies. Attempts to significantly prevent or reduce these results after substantial brain injury through various approaches to early intervention have been largely disappointing. Physical therapy after the discharge of ICU does not prevent cerebral palsy; a more global intervention of early childhood development does not prevent mental retardation. These main results will probably be significantly reduced only by the primary prevention of prematurity itself. However, it should be noted that, with modern neonatal intensive care, the vast majority of VLBW survivors and even ELBW are not left with a major neurodeveloped disability. And, more importantly, the increase in survival in recent years has not led to an increase in the rate of significant deterioration, even in the lower weights of birth. Instead, neurodevelopmental and neurobehavioral disorders "minor" remain frequent among survivors and become increasingly evident as follow-up populations age. Because these multiple brain dysfunctions increase in incidence as the birth weight and gestational age decrease, they have become especially frequent with the increased survival of the "small and sick micro-preemies". Forty to 50 percent of VLBW survivors and 60-70% of ELBW survivors will experience variable combinations of temperament problems, linguistic delays, fine motor deficits, visual-motor dysfunction, sensory integration dysfunction, social incompetence, emotional immaturity, border intelligence, attention deficits, learning disorders, and ultimately decreased school performance. In the hundreds of long-term follow-up studies conducted through multiple domains of development, a consistent theme arises: VLBW groups, premature children significantly lower and perform more badly than normal-weight socio-economic groups of birth, long-term children. These regular differences persist even when relatively "clean" groups of VLBW children experienced mild neonatal disease are examined, free from major or moderate impediments, and reside in appropriate breeding environments. It definitely seems that, in addition to the most obvious brain insults of bleeding, hypoxia/ischemia and infection, there is often a interference with the complex processes of early brain development and a resulting neurodeveloped price to pay associated with prematurity. These common "minor" neurodeveloped disorders are not necessarily less in terms of their negative impact on the functional abilities of life, including learning, socialization, work and living independently. As the high prevalence of these brain dysfunctions among VLBW survivors has been extensively realized, the corresponding interest in possible preventive or measurable interventions has naturally increased. The first place to look, logically, has been the ICU environment. The history of the development of mental intervention provided in the nursery of special care is one of initial enthusiasm, gradual physiological understanding based on evidence, and eventual complete investment of focus. At first, LBW, the premature baby was essentially considered a long-term deficient baby who needed "child stimulation" activities to bridge the development gap. As a result, early intervention efforts tended to consist of a multimodal variety of manipulations of the kindergarten environment, including tactiles combinations (massage, brushed), kinesthetic-vestibular (rocking, swinging beds), hearing stimulations (talking, music boxes), and visuals (mobile, shiny decoration). Since small controlled studies generally do not convincingly identify an optimal approach, the nurseries stayed to choose and choose for themselves. 15 to 20 years ago important data began to emerge on the fragility of the recovered premature baby and its susceptibility to the stresses of neonatal intensive care. It became clear that intrusive procedures, repetitive management and other "overstimulation" frequently caused interference with the self-regulation and stability of the autonomic nervous system to the point of apnea, bradycardia, hypotension and reduction of the flow of brain blood. This new information clearly indicates that the existing conceptualization of the needs of the premature baby must be re-evaluated. Could ICU's standard practices that save lives with their ecology from the ongoing disruption of childhood day rhythms and sleep-wake cycles really be detrimental to long-term brain function? The predominant approach to the environmental issue of ICU in recent years has evolved to a dramatic different orientation than the original. Through the work of Dr. Heidi Als and others have defined the concept of individualized development care and is increasingly applied in intensive care nurseries in the United States and around the world. At the core of this philosophy is the somewhat revolutionary idea that the unstable premature baby mainly needs time and space to recover and be handled carefully. This "child protection" approach is markedly contrasted with previous stimulating attitudes. Individualized development care requires a deep recognition of brain development by gestational age, as well as evaluation techniques to determine neurological preparation for interactions and interventions of each baby. It includes specific details such as a "minimum manipulation" protocol tempered to the receptivity issues of the baby, facilitative positioning, skin contact (canguro) and a radical restructuring of the ICU to reduce excessive pollution of light and noise. Sensibly try to consider each baby as a unique development and need careful "brain care." A number of studies have evaluated development care with short-term positive preliminary results, such as short-term respiratory, weight improvement and reduced hospitalization duration. At least, it makes good sense and human care for VLBW sick children, their families and their NICU providers. However, even if it is applied optimally, development care will probably not eliminate the many neurodeveloped dysfunctions associated with prematurity. The development interventions of the LBW, premature infants after the day-care download have also been investigated. The broadest and most ambitious of these is the Programme for Child Health and Development (PIHDP). The IHDP is a national, multisite randomized clinic trial of a related group of early interventions designed to optimize the long-term school outcomes and minimize the developmental and behavioural sequelae of prematurity. In the mid-1980s, approximately 1,000 LBW children in eight colleges were randomized to an intervention or follow-up group before leaving the hospital. The population studied was stratified by birth weight with one third of the babies (heavier group) with a birth weight of between 2,001 and 2,500 grams and two thirds (light group) with a weight of 2,000 grams or less at birth. The "package" intervention was guided by a written curriculum of early development activities and included regular home visits, daily assistance to a special development centre, and parent group meetings focused on topics during the first three years of life. Both groups received a close follow-up evaluation, support for social services as necessary and the referral of specific therapies if necessary. While the formal set of interventions concluded at 3 years of age, the study population has continued to be followed and evaluated in multiple areas over 8 years. More than 90% of the study families are still available for long-term follow-up. The initial results at the end of the study interventions seemed quite positive. Children in the intervention group had significantly higher intelligence (IQ) scores and significantly less behavioral problems. Obviously, these first results were acclaimed as reducing the impact of low birth weight and prematurity. But as with early interventions for socio-economically disadvantaged children, the large differences in intellectual coefficient quickly decreased over time. The most disconcerting of all was the observation that, as the birth weight and gestational age decreased, also the difference in the intellectual coefficient measured between the intervention and follow-up groups. Weightweight children at birth lighter did not show group differences in any development or behavior parameter, including early academic skills, at age five and eight. Children with higher birth weight maintained small and significant group differences in the IQ and language at these later ages, based on the increased impact of intervention on children and families with high environmental risk. In sharp contrast, even these extensive high-quality interventions seem unable to produce a significant development increase at the early age of school or to prevent the deterioration of these premature children at the highest biomedical risk of brain dysfunction. A final assessment of the monitoring of the population of IHD in the late secondary school is currently planned to investigate the possibility of long-term intervention in the academic and social role. So what have we really learned and where are we going from here? It must be clear to all now that prematurity, especially extreme prematurity, results in a substantial intrinsic risk for the developing brain even in the absence of excessive neuroimaginous anomalies. This risk is multifactorial and often subtle, but it manifests itself in long-term deficits in various life skills. If this fragile baby was also prenatally exposed to potentially eliminating substances and eventually goes to a vulnerable and chaotic environment, then the risks to the relevant development and behavior are multiplied. We are gradually learning ways to interrupt this cycle. We need to apply more fully what we already know. Public health efforts to reduce the incidence of low birth weight and prematureity should be conceptually and financially supported. The vascular and neurochemical risks of tobacco, alcohol, cocaine, marijuana, methamphetamine and other substances adverse to the fetal brain should be publicly emphasized instead of exonerating. Neonatologists should pay at least as much attention to the premature brain as to the premature lung and increase the knowledge applicable in areas such as brain blood flow and neonatal nutrition. The philosophy and practices of individualized development care should be widely applied in ICUs, as the birth and care of children in the long term had been humanized several decades ago. Finally, while early intervention efforts targeting LBW, premature infants in the early years of life have not proved to be as beneficial as they expected to prevent negative results associated with biomedical risk, it is increasingly clear that these comprehensive interventions can significantly improve language, learning and behavioral outcomes associated with environmental risk. However, in order to be fully effective these interventions must have a high level of intensity and duration (i.e., starting early in life and continuing in the early years of school), actively involve families and help them solve overwhelming life needs, and be carried out by competent and committed persons who receive adequate compensation for this important work. This is a high order and an unfulfilled challenge for policymakers and all of us. Are we as a society, both collective and individual, to it? Connect with NursingCenter of Nursing on social media to learn about latest news and special offers Find your next job with JOBSPLUSCE Nursing Resources About NursingCenterConnect with NursingCenterConnect with us on Facebook, Twitter, Linkedin, YouTube, Pinterest, and Instagram.© 2021 Wolters Kluwer Health, Inc. and/or its subsidiaries. All rights reserved. - - - - - v7.7
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to enable Javascript in your browser. Baby furniture 19 Items 19 Items
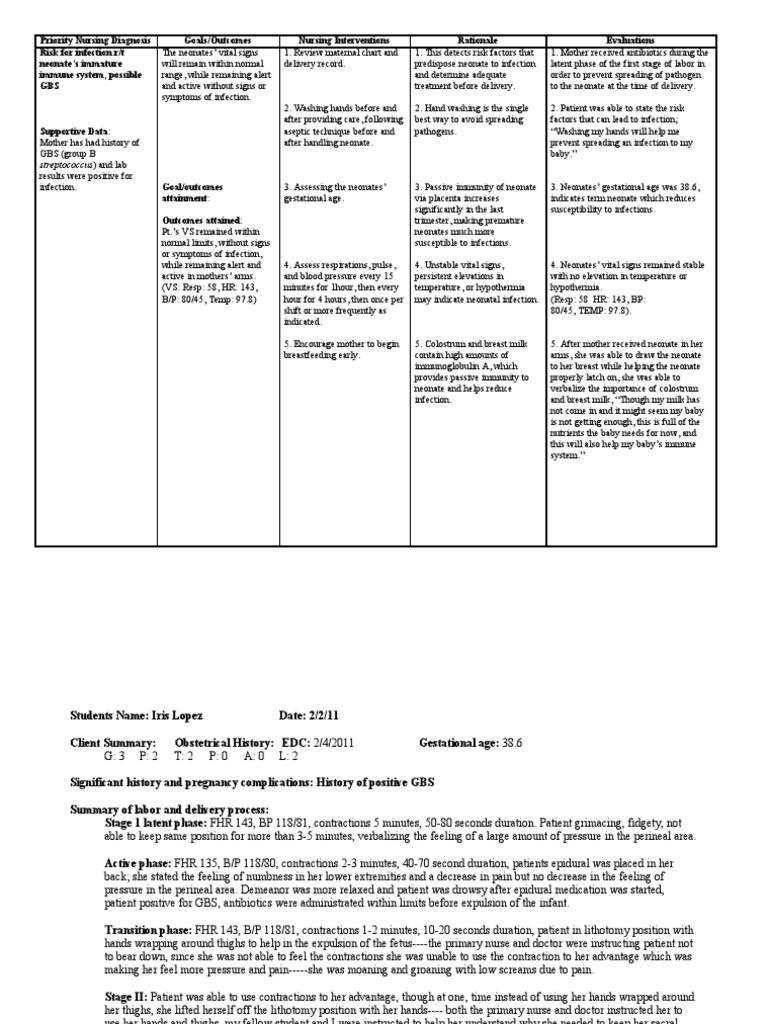
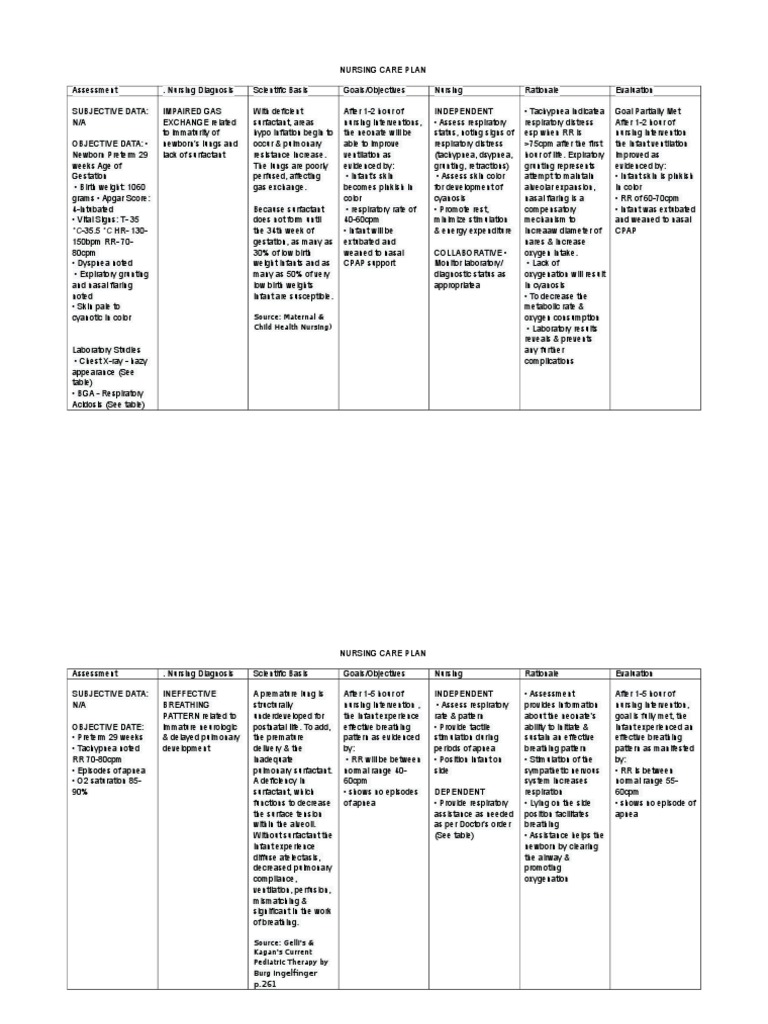
![PDF] A Premature Baby's Nursing Care Plan | Semantic Scholar PDF] A Premature Baby's Nursing Care Plan | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/50ff67850b959b4cecc23bf954636b94f2b0dacd/5-Table1-1.png)
PDF] A Premature Baby's Nursing Care Plan | Semantic Scholar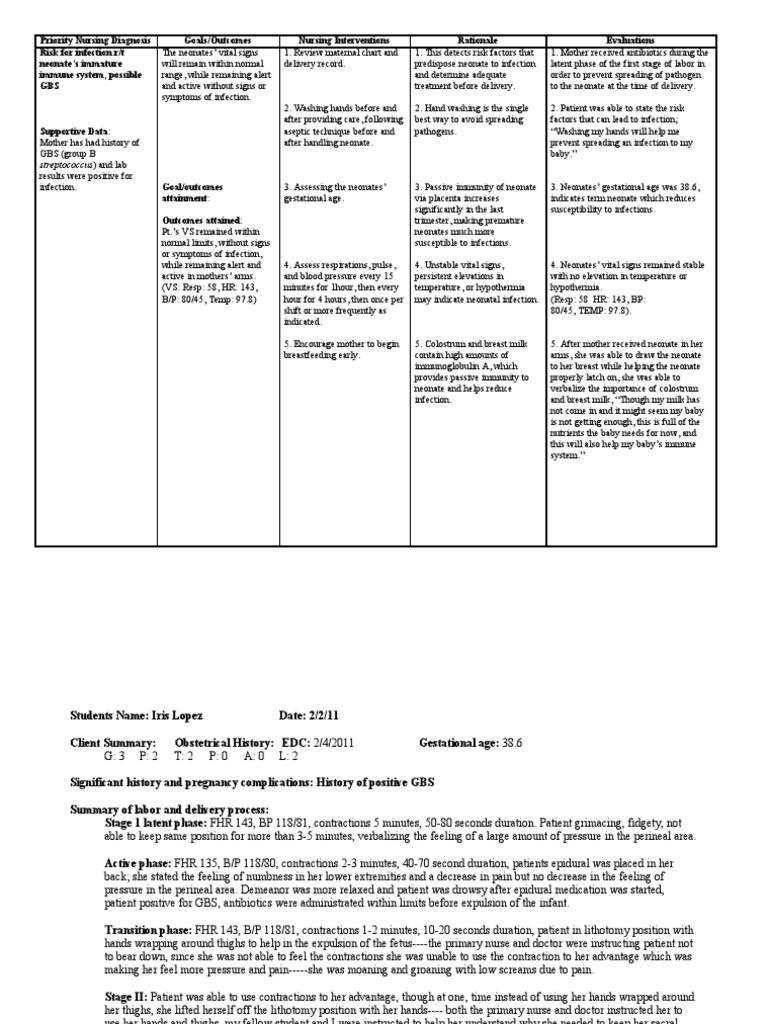
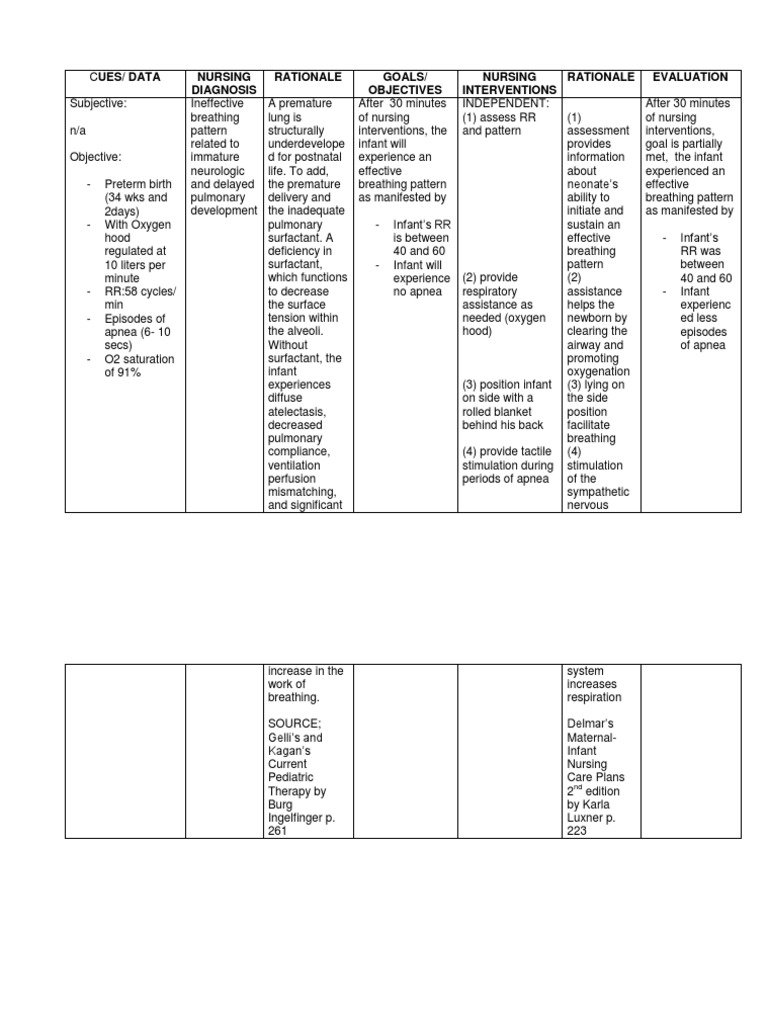
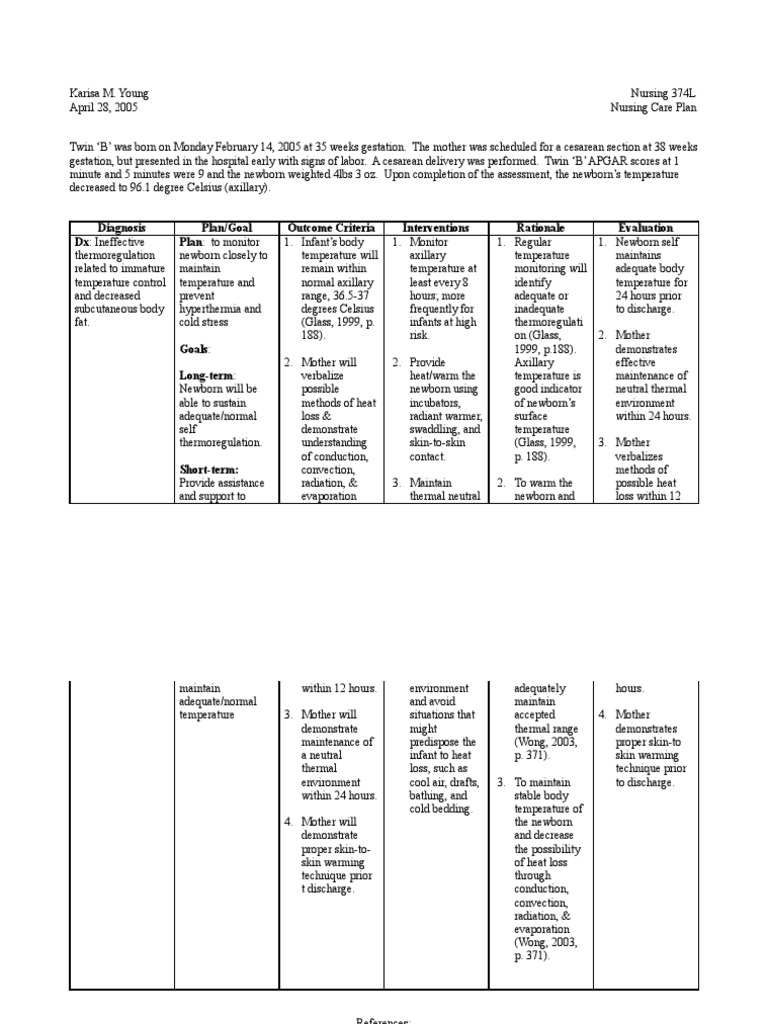
Premature Baby Nursing Care Plan Nurse Lab - Newborn baby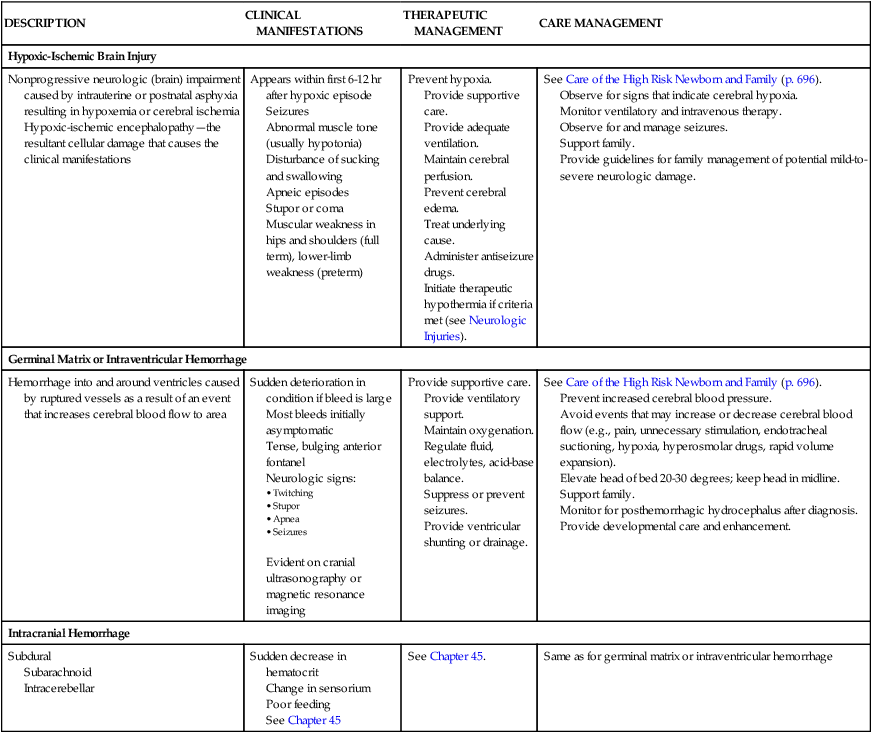
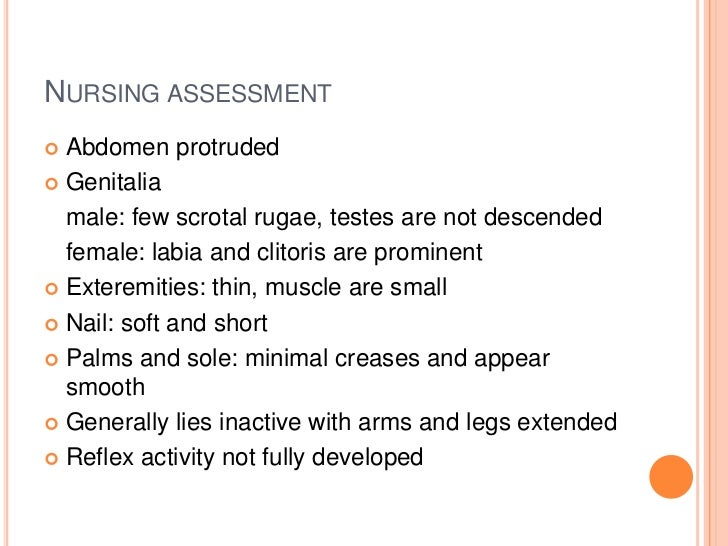
The High Risk Newborn | Nurse Key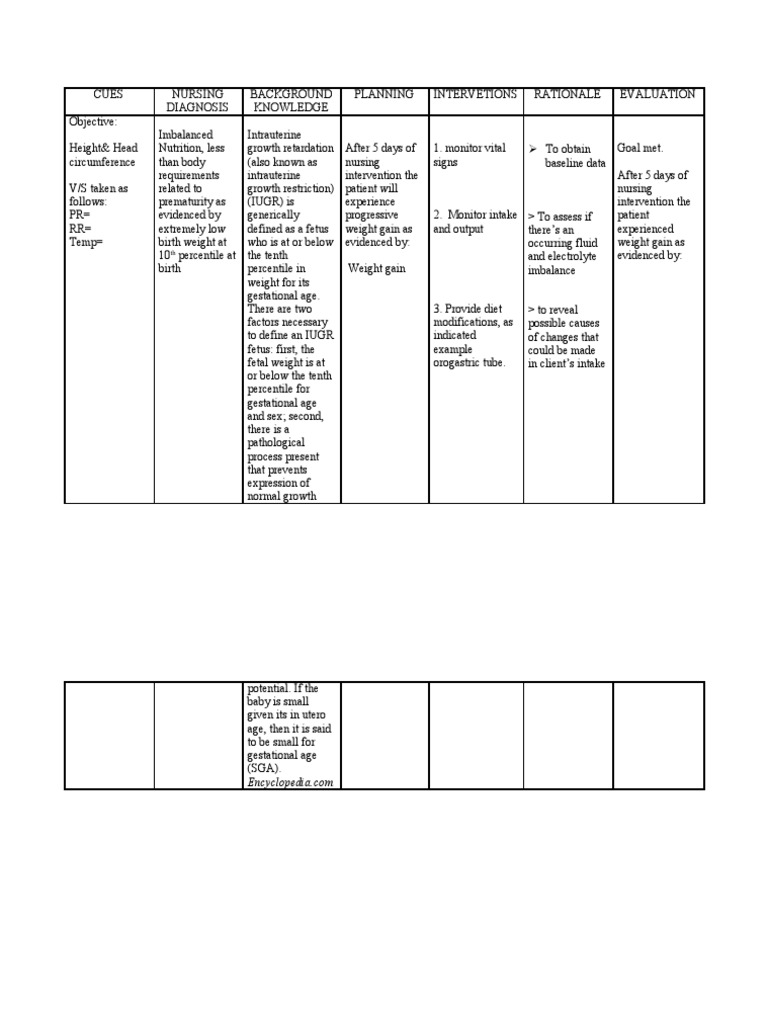
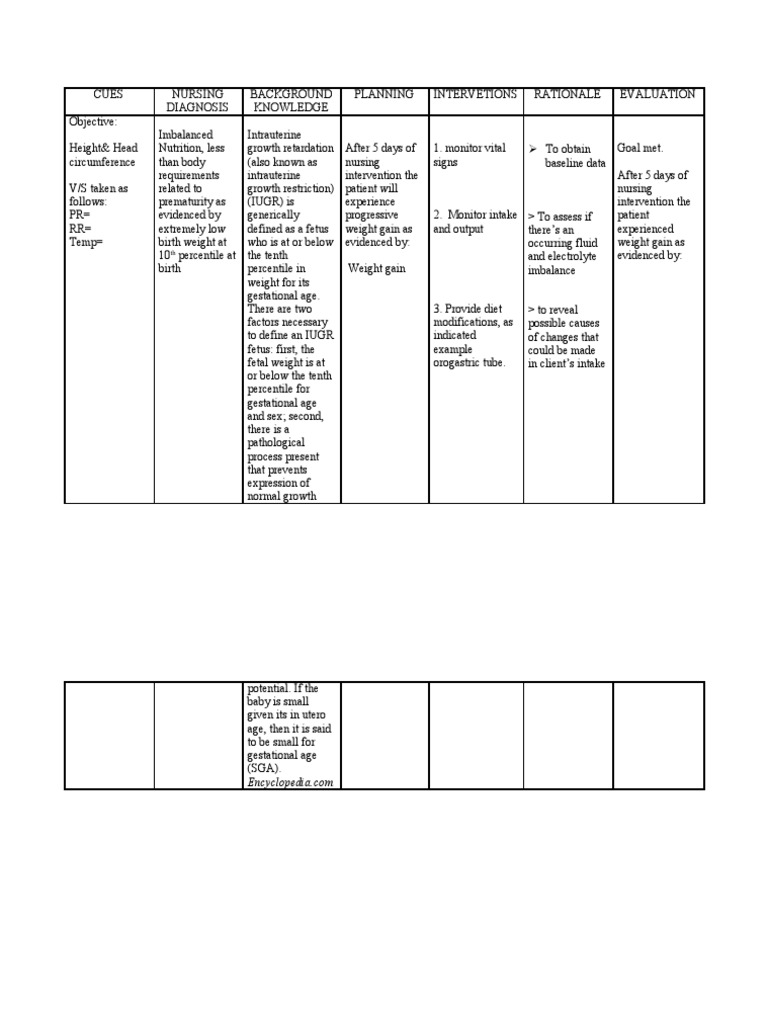
Nursing Care Plan For Premature Baby With Low Birth Weight - Newborn baby
Hypertension Nursing Care Plan Scribd - Hypertension Nursing Care Plans
Nursing Care Plan For Newborn Baby - newborn baby
Nursing Care Plan for Newborn Baby (Page 1) - Line.17QQ.com
83 Best Nursing care plans ideas | nursing care plan, nursing care, care plans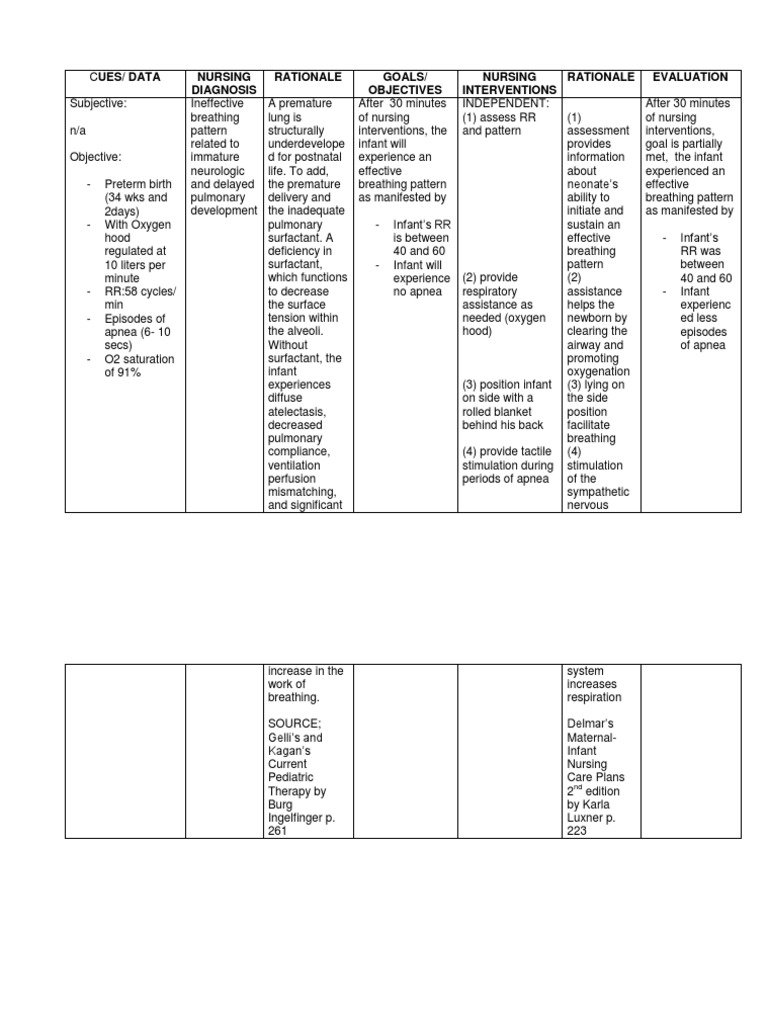
Ncp Newborn | Infants | Preterm Birth
Diabetic Foot Ulcer Nursing Care Plan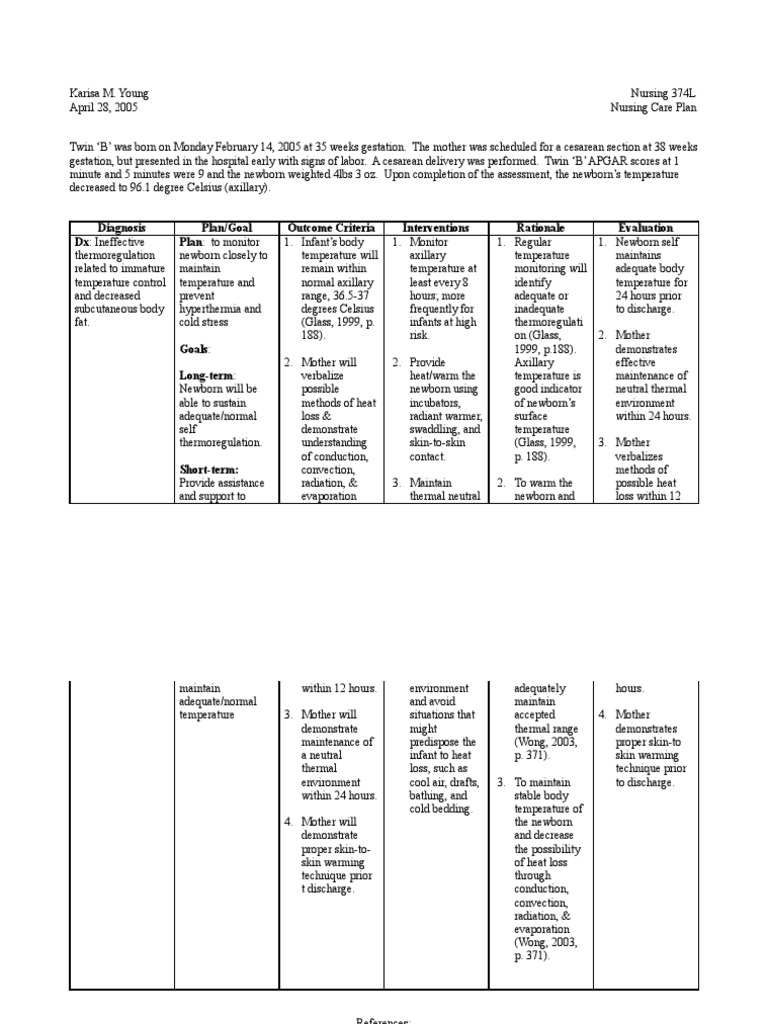
Care Plan For Newborn Baby - Newborn baby
Home Visiting Programs for Parents of Preterm and Low Birth Weight Babies | Download Table
Hypertension Care Plan Nursing Diagnosis
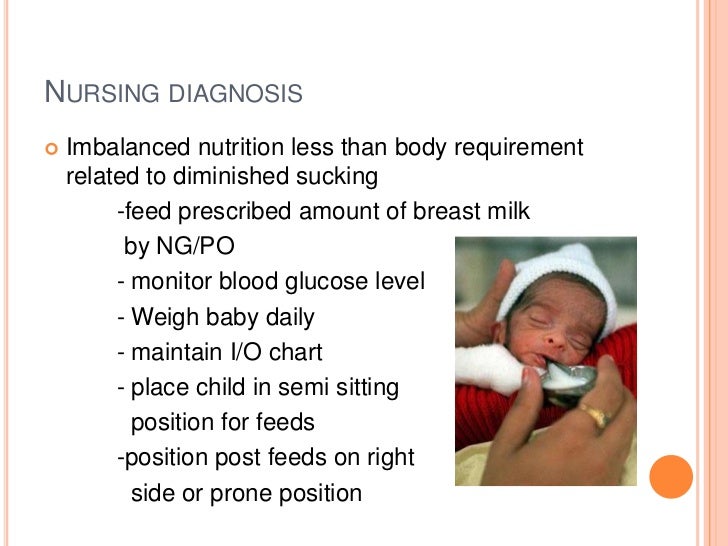
Nursing management of low birth weight(lbw) babies![nursing care plan for low birth weight baby for 2021, [Printable and Downloadable] - Lomen nursing care plan for low birth weight baby for 2021, [Printable and Downloadable] - Lomen](https://onlinelibrary.wiley.com/cms/attachment/bb573827-cf23-4b55-9745-847b5f55d047/jogn1338-fig-0001-m.jpg)
nursing care plan for low birth weight baby for 2021, [Printable and Downloadable] - Lomen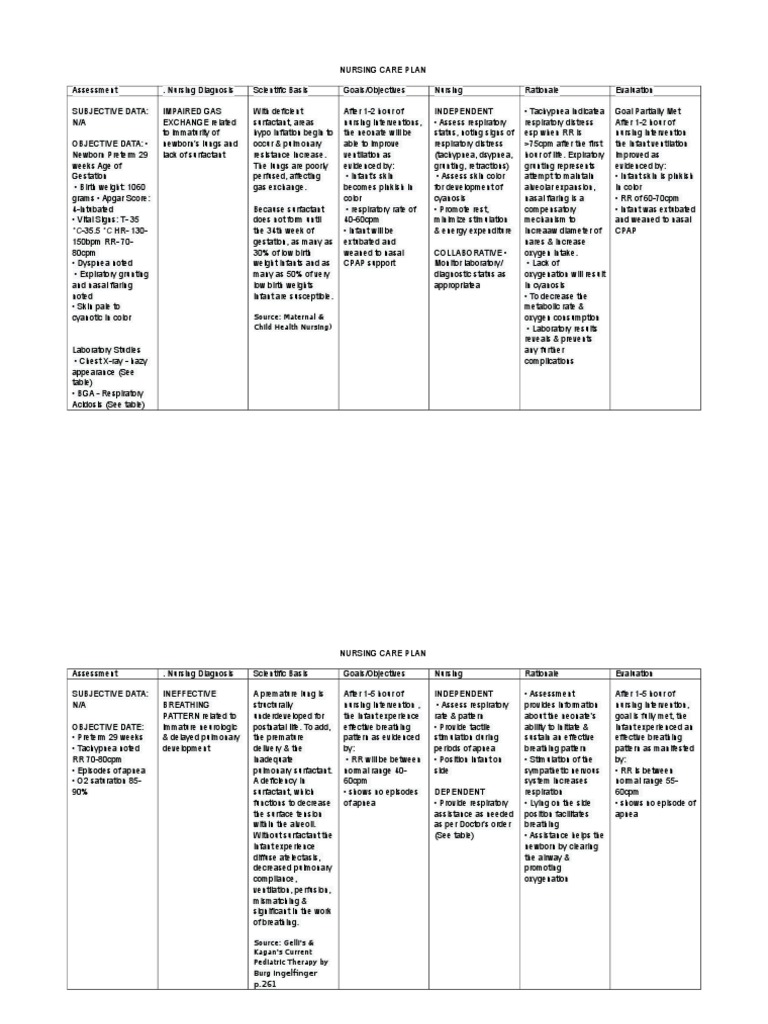
Nursing Care Plan | Breathing | Neonatal Intensive Care Unit
Nursing Care Plans For Newborn Baby - Newborn baby
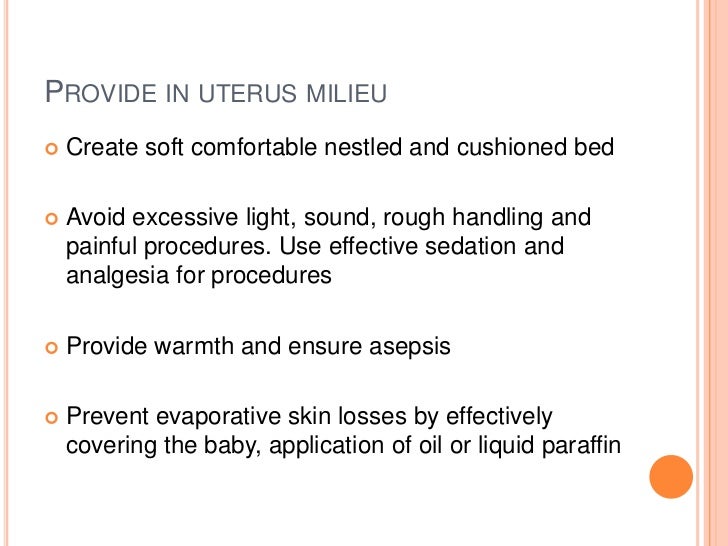
Nursing management of low birth weight(lbw) babies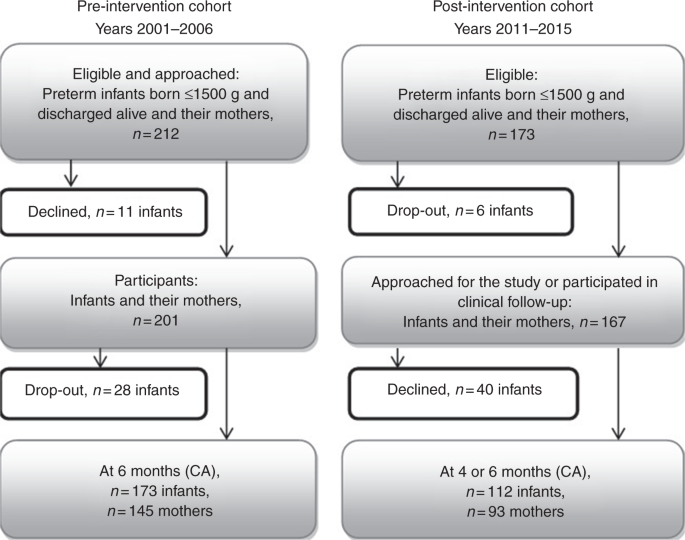
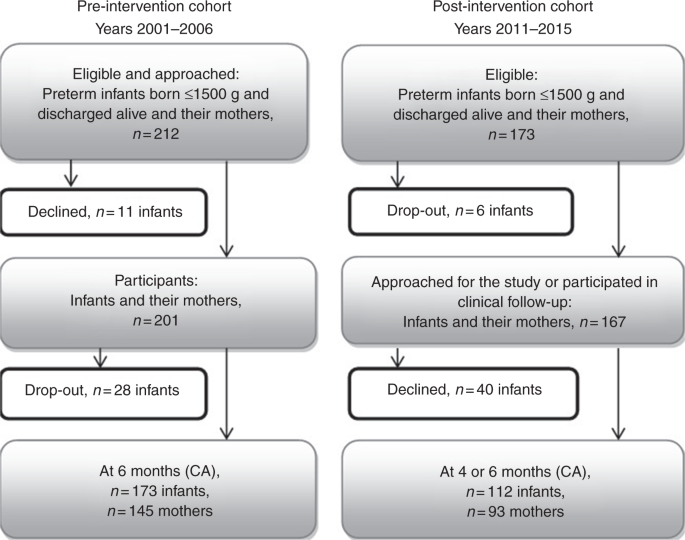
An educational intervention for NICU staff decreased maternal postpartum depression | Pediatric Research
Fluid Volume Excess Nursing Diagnosis & Care Plan - Nurseslabs
NCLEX: Health Promotion and Maintenance; Nursing Care of the Childbearing Family - Brilliant Nurse®
Nursing management of low birth weight(lbw) babies![62062942 Nursing Care Plan AML - [DOCX Document] 62062942 Nursing Care Plan AML - [DOCX Document]](https://demo.vdocuments.mx/img/378x509/reader024/reader/2020123116/54517f9eb1af9f7f248b487c/r-1.jpg)
62062942 Nursing Care Plan AML - [DOCX Document]
What is a nursing care plan for fever? - Quora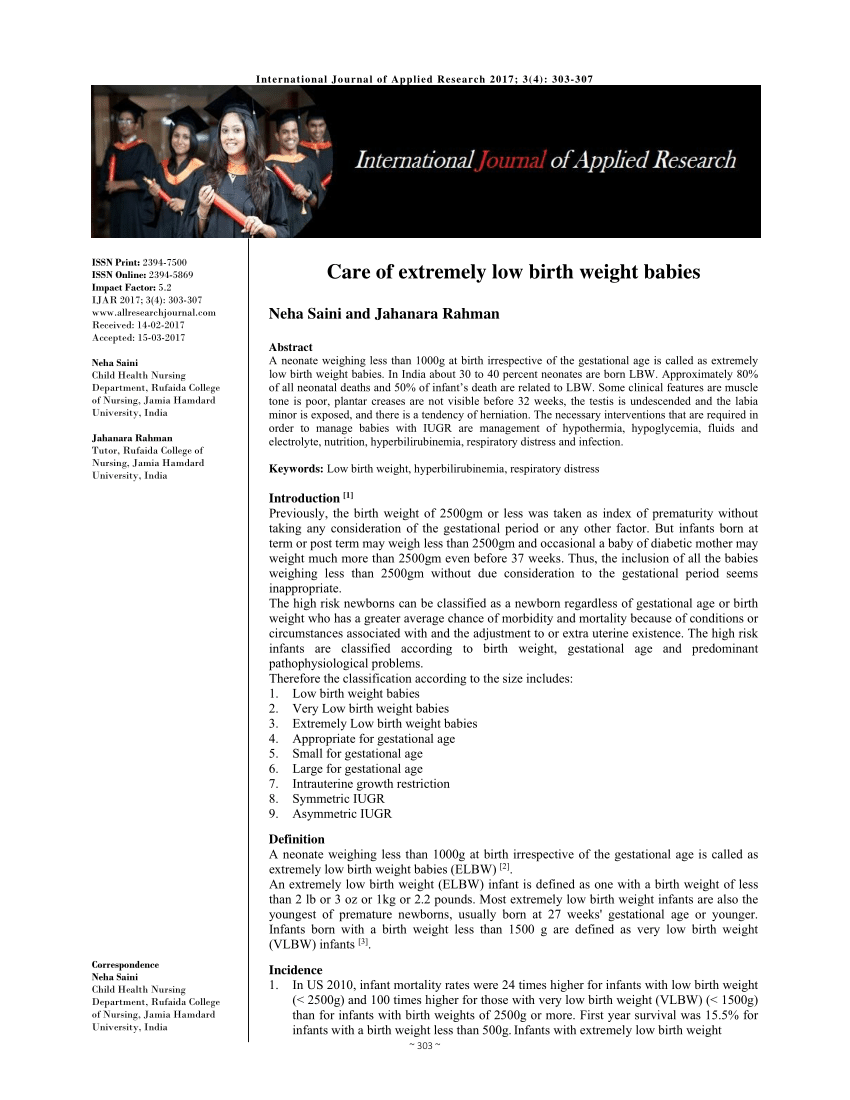
PDF) Care of extremely low birth weight babies
83 Best Nursing care plans ideas | nursing care plan, nursing care, care plans
Nursing management of low birth weight(lbw) babies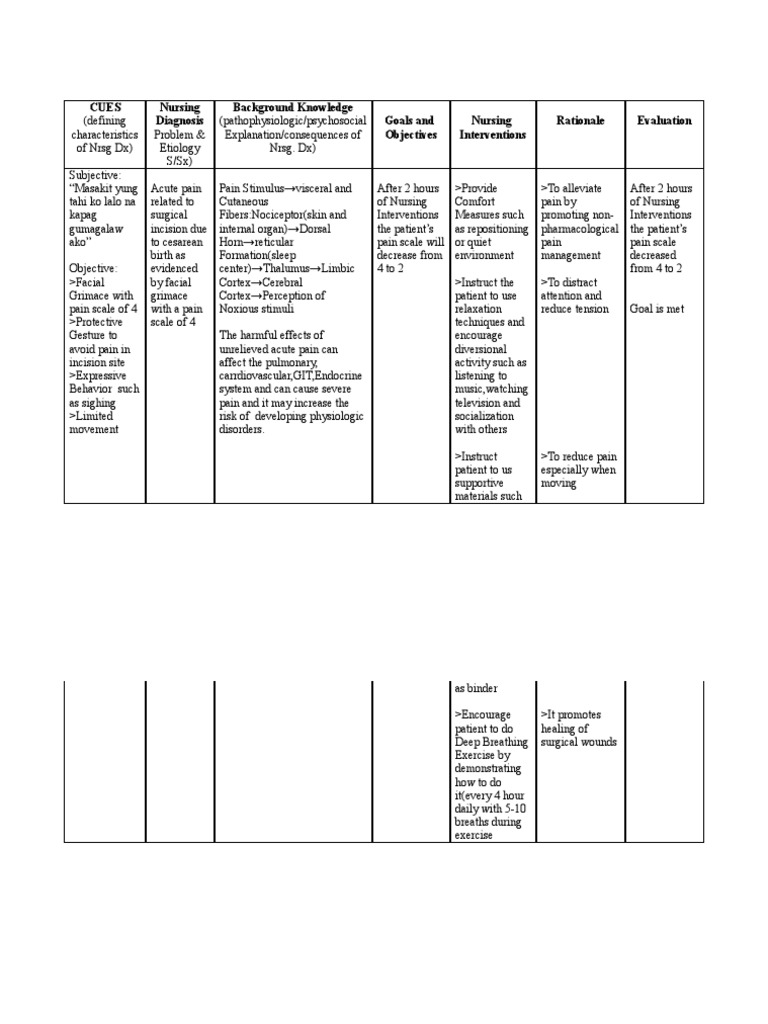
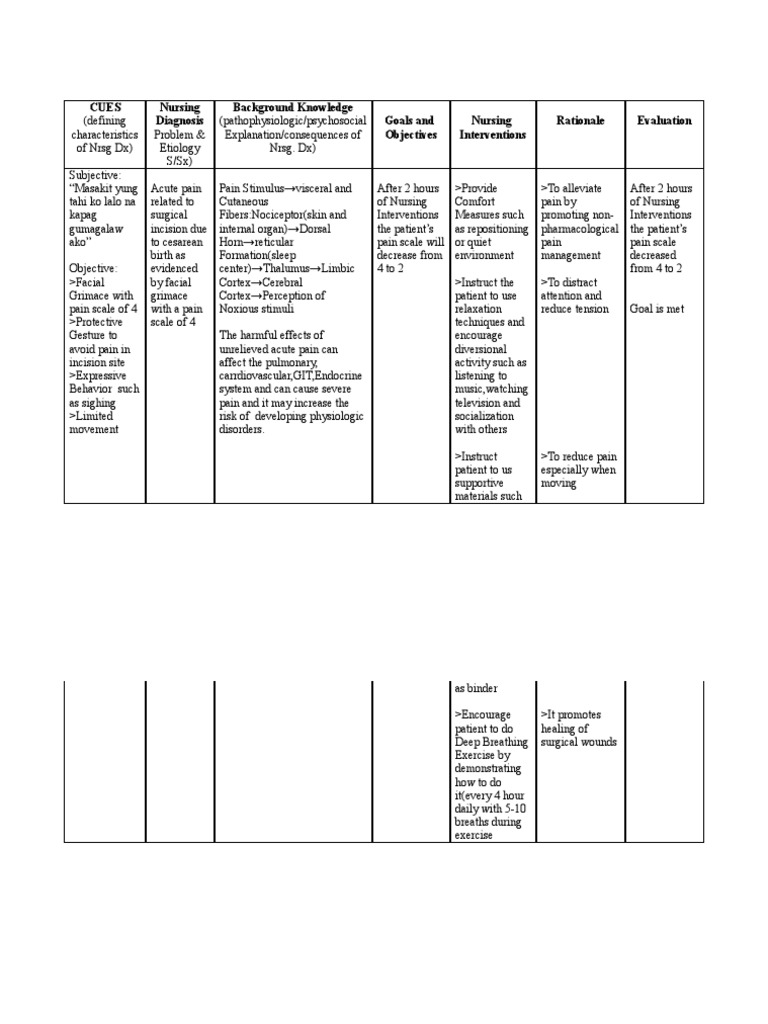
Nursing Care Plan (acute pain for ceasarean birth) HYPOTHETICAL | Pain | Wound
From care plan to concept map: A paradigm shift - ScienceDirect
Cancer Nursing Care Management and Study Guide for Nurses
NCLEX: Health Promotion and Maintenance; Nursing Care of the Childbearing Family - Brilliant Nurse®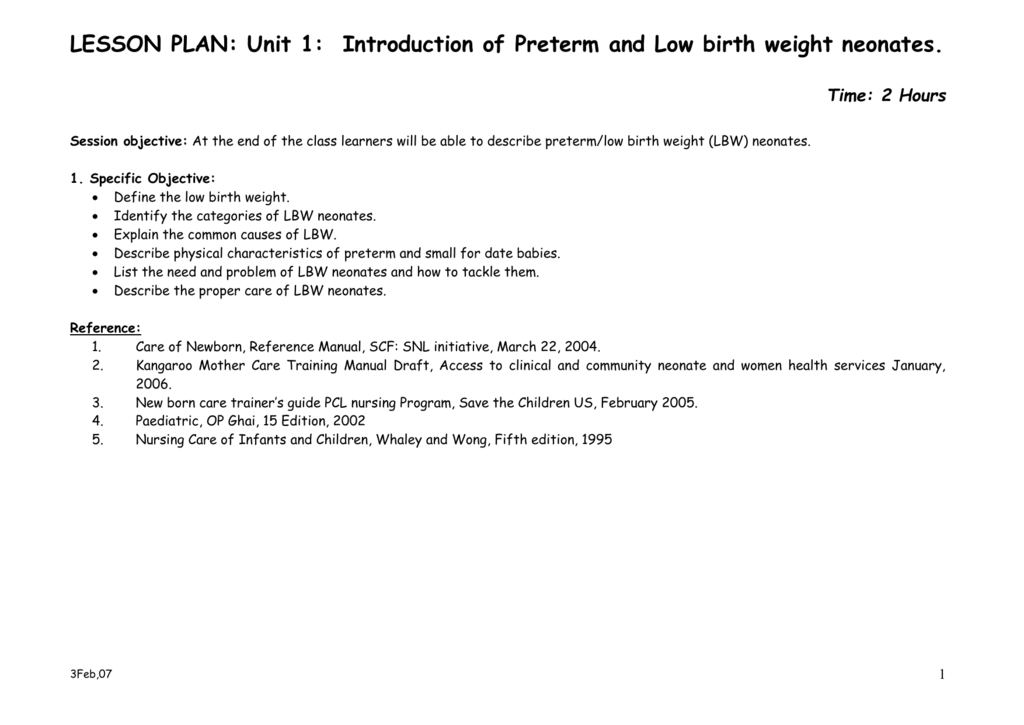
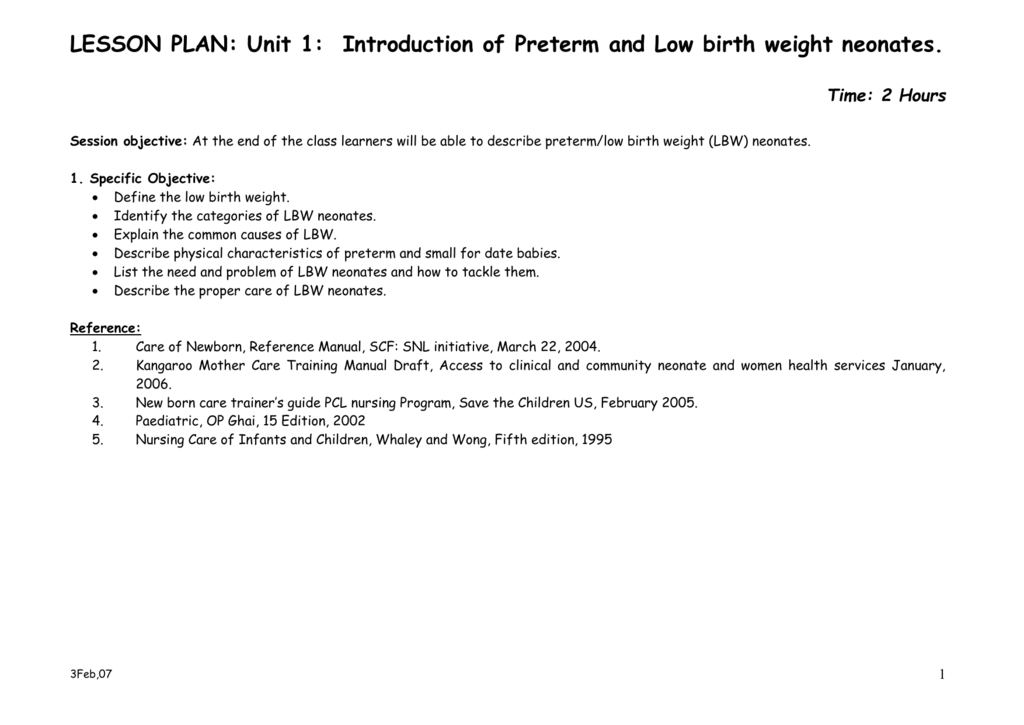
LESSON PLAN : Unit 1: Introduction of Preterm and Low birth weight.jpg)
Clinical Guidelines (Nursing) : Neonatal hypoglycaemia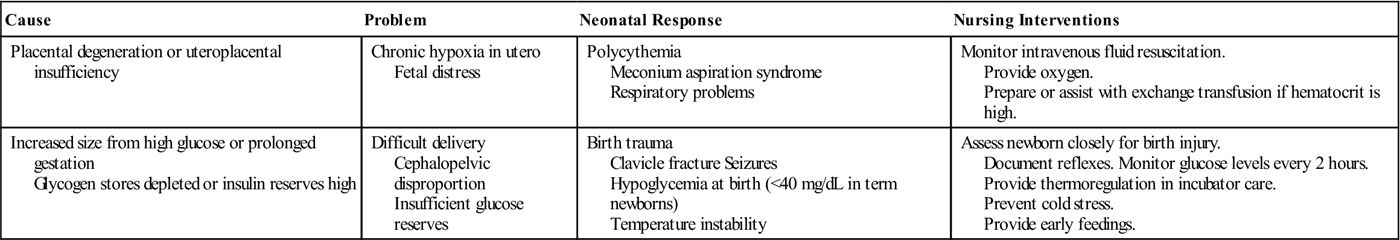
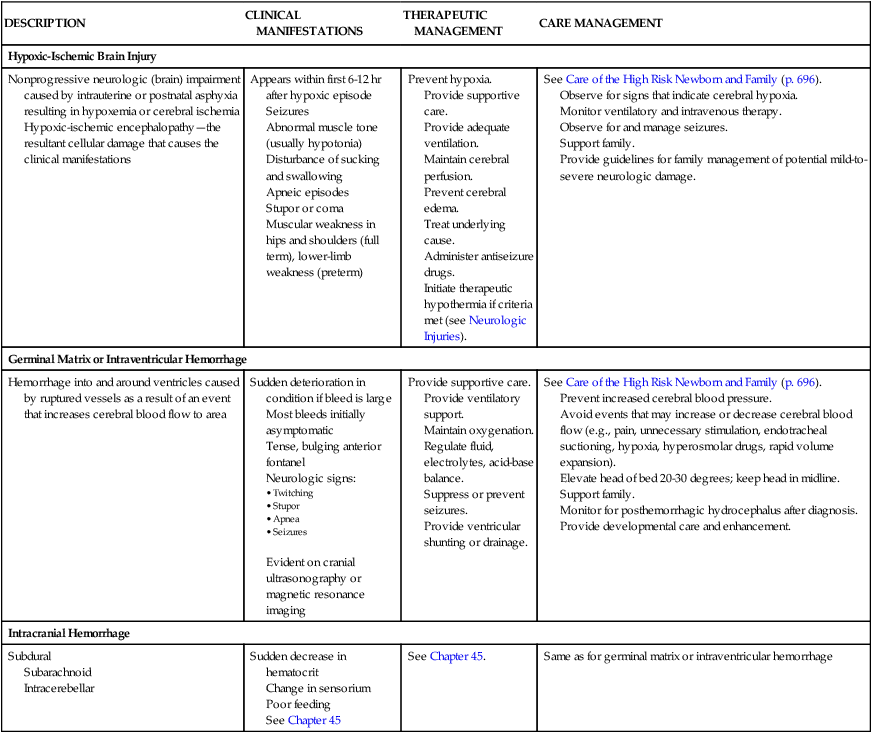
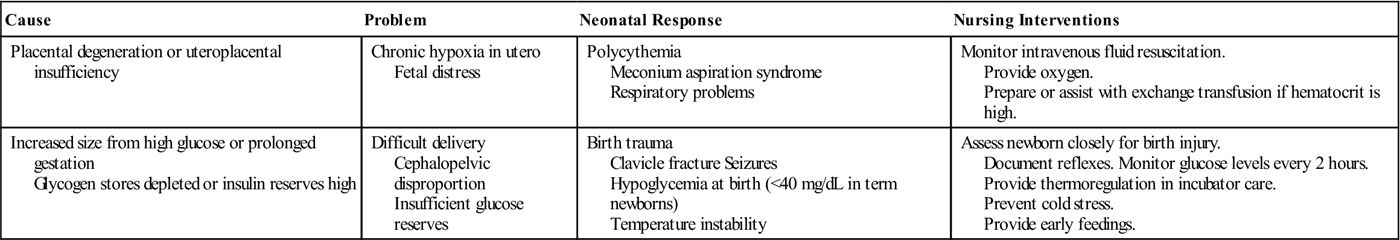
15. The Newborn at Risk: Conditions Associated with Gestational Age and Development | Nurse Key
6 Hysterectomy and TAHBSO Nursing Care Plans - Nurseslabs
Nursing Care Plan and Diagnosis for Imbalanced Nutrition: More Than Body Requirements | Nanda Nursing Interventions and Outcomes Goals
13 NCP ideas | nursing care plan, nursing care, nursing diagnosis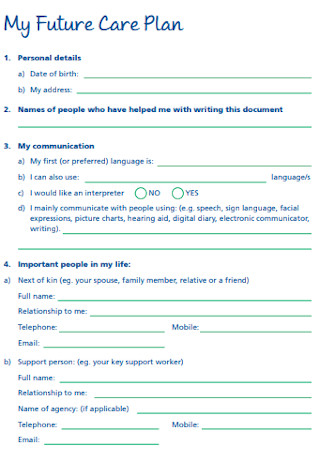
42+ Sample Care Plan Templates in PDF | MS Word
Ineffective Breastfeeding: Nursing Diagnosis & Care Plan - Health Conditions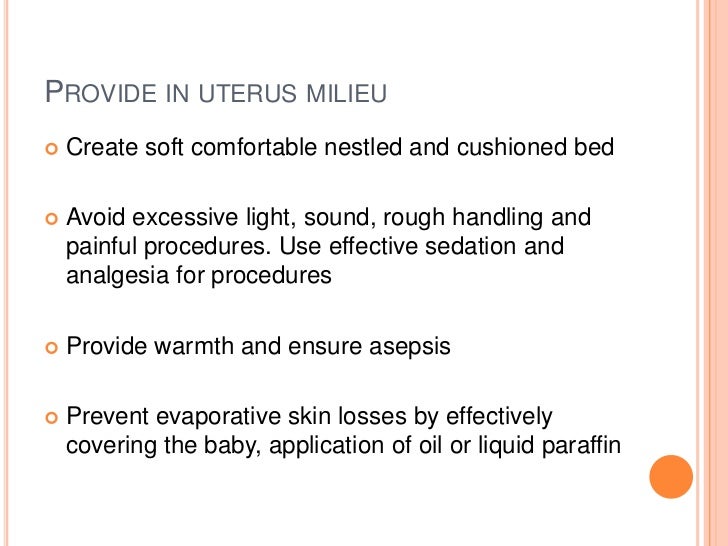
Nursing management of low birth weight(lbw) babies
 Nursing Care Plan For Newborn Baby - Newborn baby
Nursing Care Plan For Newborn Baby - Newborn baby![PDF] A Premature Baby's Nursing Care Plan | Semantic Scholar PDF] A Premature Baby's Nursing Care Plan | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/50ff67850b959b4cecc23bf954636b94f2b0dacd/5-Table1-1.png)







![nursing care plan for low birth weight baby for 2021, [Printable and Downloadable] - Lomen nursing care plan for low birth weight baby for 2021, [Printable and Downloadable] - Lomen](https://onlinelibrary.wiley.com/cms/attachment/bb573827-cf23-4b55-9745-847b5f55d047/jogn1338-fig-0001-m.jpg)



![62062942 Nursing Care Plan AML - [DOCX Document] 62062942 Nursing Care Plan AML - [DOCX Document]](https://demo.vdocuments.mx/img/378x509/reader024/reader/2020123116/54517f9eb1af9f7f248b487c/r-1.jpg)



.jpg)




Posting Komentar untuk "nursing care plan for low birth weight baby"